LEARNING OBJECTIVES
At the end of this module the staff will be able to:
💦 understand the therapeutic intent of treatment
for hematological malignancies
💦describe commonly used treatment options and their mechanism of action
💦 identify common side effects and complications of cancer treatments
TREATMENT AND MANAGEMENT
The purpose of treatment is known as the treatment intent. This can be curative, palliative or active surveillance.
FACTORS THAT AFFECT TREATMENT DECISIONS
There are several factors that may affect treatment options for patients with a hematological malignancy. These are considered prior to the initiation of treatment and include:
TYPES OF TREATMENT
There are a variety of treatment options commonly utilized in the management of hematological malignancies.
These treatment options may be used alone or in combination as part of a patient's treatment plan.
Examples include:
Surgery is not a common treatment option in the management of haematological malignancies due to the nature of the disease and blood disorders such as excessive bleeding or clotting further complicating surgical procedures.
Anti-cancer drug treatment overview
Anti-cancer drug therapy is used in most treatment plans for hematological malignancies.
Anti-cancer drug therapies used for hematological malignancies include:
Different drug classes may be used alone or in combination( called combination therapy) as a part of the treatment protocol.
Combination therapy assists in achieving maximum cell kill while avoiding additional toxicities.
The time between treatment cycles and future scheduling of treatment is very important.
Cancers are more likely to respond to treatment if there are no significant delays between planned cycles.

Let’s take a closer look at chemotherapy, targeted therapy and immunotherapy and learn how they are used in the treatment of haematological malignancies.
Chemotherapy is often called ‘chemo’ and referred to as ‘cytotoxic’.
The word cytotoxic is of Greek origin and translates to
Cyto = cell and toxic = kill
This underpins the definition of chemotherapy which works by killing or inhibiting the growth of rapidly dividing cells, thereby reducing the ability of cancer to grow or spread. Generally, chemotherapy does this by interfering with the cell cycle. The cell cycle is a series of phases a cell takes to divide into two new cells. Chemotherapy can affect one or more of these phases.
Targeted cancer therapies are medicines that interfere with specific molecules (‘molecular targets’) involved in cancer cell growth and survival. Molecular targets may be genes, receptors, mutations or proteins. Patients undergo molecular profiling at the time of diagnosis to test for the presence of these targets or markers.
Examples of targeted therapies you may come across in your practice, and their molecular targets include:
💥 Rituximab and Obinutuzumab - work by binding to the CD20 antigen found on the surface of normal and malignant B-lymphocytes.
💥 Imatinib - works by blocking a group of enzymes called tyrosine kinases from sending signals that tell malignant cells to continue to grow and spread. Without this signal, malignant cells die.
Targeted therapies differ from standard chemotherapy in several ways, such as:
💢targeted therapies act on specific molecular targets, whereas chemotherapy tends to act on all rapidly dividing cells (normal and malignant cells). In this way, targeted therapy causes less damage to normal, healthy cells.
💢 targeted therapies are often cytostatic (they block cancer cell proliferation) whereas chemotherapy is cytotoxic (they kill cancer cells).
Targeted therapies can be used alone or in combination with chemotherapy drugs in the treatment of haematological malignancies.
Immunotherapy, in the cancer setting, is any medicine or treatment which boosts the ability of the patient’s immune system to initiate an effective response against cancer.
Types of Immunotherapy
The classification of medications can often overlap and fall into several different categories, e.g. monoclonal antibodies are often categorized as immunotherapy as well as targeted therapy.
1. Immune checkpoint inhibitors

These drugs take the ‘brakes’ off the immune system, helping T-cells to recognize and kill malignant cells. Immune checkpoint inhibitors are becoming more widespread in the treatment of hematological diseases.
For example, pembrolizumab is approved for the treatment of Hodgkin and non-Hodgkin lymphoma. Pembrolizumab blocks the PD1 pathway, an immune pathway which cancer cells can use to hide from the immune system.
2. Immunomodulators (IMiDs)
The way IMiDs affect the immune system is not entirely clear, but they have been found to be useful in the treatment of multiple myeloma. The first of these medicines, thalidomide, caused severe birth defects and fatalities when taken during pregnancy. Subsequent drugs, lenalidomide and pomalidomide, are presumed to have the same adverse effect. For this reason, IMiDs can only be dispensed by pharmacies registered with an access program from the manufacturer.
3. Chimeric antigen receptor T-cells (CAR T-cells)
A specialized and complex treatment in which a patient’s T-cells are engineered to launch an immune attack on the cancer cells. A sample of circulating T-cells are taken from the blood of an individual with cancer using an apheresis machine. The T-cells are genetically engineered to express a specific antigen receptor and target the specific antigen expressed on the cancer cells of the patient. The CAR T-cells are cloned in bulk and then transfused back into the patient to launch a sophisticated immune attack on their cancer.
Radiation therapy (also called radiotherapy) uses high-energy beams, such as x-rays, gamma rays, electron beams or protons to kill or damage cancer cells.
Radiation therapy is a local treatment, only affecting the areas of the body where the radiation is directed.
In the treatment of hematological malignancies, radiation therapy may be used as part of a treatment plan to achieve remission, as a palliative treatment to alleviate pain or discomfort from bony tumours (multiple myeloma) or as part of the conditioning regimen for BMT.
Anti-cancer drug therapy side effects
Side effects of cancer treatment vary from patient to patient and depend on the type of treatment given.
Chemotherapy
Chemotherapy not only affects cancer cells. It can kill or inhibit the growth of healthy cells within the body, particularly those cells that divide rapidly, e.g. bone marrow, hair follicles, cells lining the gastrointestinal tract and the reproductive organs. This can result in patients experiencing undesirable side effects and toxicities.
The side effects of chemotherapy are largely drug and dose-dependent. Some common side effects and complications of chemotherapy can include, but are not limited to:
Targeted therapy
Targeted therapy side effects depend on the type of targeted therapy administered and the body’s reaction to it.
Immunotherapy side effects are known as immune-related adverse events (irAEs). They are a direct result of the immune system being activated to launch an immune attack against cancer cells and are different from chemotherapy side effects.
Immune-related adverse events can affect any body system, present at any time during or after treatment, and be life-threatening.
Radiation therapy side effects
Most side effects from radiation therapy are ‘site specific’ or localized to the anatomical region or system being treated.
Patients will experience different side effects depending on which part of the body was treated and the dose received. Side effects may be acute or late.
Acute: Short term side effects during or within a few weeks after radiation therapy (usually temporary).
Late: Long term side effects - months/years post radiation therapy (may be permanent).
Patients receiving treatment for haematological cancers may receive radiation therapy to nodal areas in the neck, chest, abdomen and pelvis. Bony lesions may also be treated.
 |
Some of the common side effects that patients may experience when receiving radiation therapy to these areas.
People receiving radiation therapy may also experience fatigue, alopecia in the site being treated and cytopenia. There is also a chance of developing a secondary malignancy (late effect).
|
Oncological emergencies are life-threatening complications that can occur as a result of cancer or its treatment.
Below is a list of some oncological emergencies that can occur when patients are receiving or have recently undergone cancer treatment for haematological malignancies. These require immediate medical attention.
 |
Febrile neutropenia can occur if a patient is neutropenic (has a low level of neutrophils, a white blood cell responsible for fighting infection) and develops a fever and other signs of infection.
|
Febrile neutropenia is defined as a temperature of 38.0°C or greater and neutrophil count of less than 0.5 x 109/L, or less than 1.0 x 109/L and predicted to fall to lower than 0.5 x 109/L.Febrile neutropenia is a medical emergency and can result in significant morbidity and death.
1. Importance of patient education (Watch video)
2. Importance of early presentation and recognition (Watch video)
3. Importance of early intervention (Watch video)
TLS can occur spontaneously, during or after cancer treatment when there is bulky disease (commonly seen in patients with lymphoma). It usually occurs in the first cycle of chemotherapy and is caused by the death or “lysis” of large numbers of cancer cells resulting in metabolic abnormalities such as elevated uric acid, potassium and phosphate levels. This can lead to renal failure, cardiac arrhythmias, seizures, neurological complications and potentially sudden death.
When tumour cells die, their cell contents including phosphate, potassium and nucleic acids are released into the blood stream.
Cancer therapies can cause the death of a large number of cancer cells, resulting in large amounts of these substances being released into the bloodstream.
This mass cell death causes the levels of phosphate, potassium and nucleic acid in the blood to rise causing a range of potential toxicities including:
💥 renal failure
💥 cardiac arrhythmias
💥 seizures
💥 neurological complications
💥 and death due to multi-organ failure.
This is called tumour lysis syndrome. Tumour lysis syndrome most commonly occurs after commencing systemic anticancer treatment but can also occur spontaneously in highly proliferative diseases or following radiation therapy.
Tumour lysis syndrome can develop rapidly, result in serious and potentially life threatening consequences if not corrected and is considered an oncological emergency.
Risk Factors:
Tumour lysis syndrome most commonly occurs after commencing systemic anticancer treatment but can also occur spontaneously in highly proliferative diseases or following radiation therapy.
TLS can develop rapidly, result in serious and potentially life threatening consequences if not corrected and is considered an oncological emergency.
Signs and symptoms
Onset of symptoms is most common within 12 to 72 hrs. of initiating systemic anticancer treatment, however, can occur before commencing treatment.
The clinical presentation of TLS is often representative of the manifesting metabolic disturbances, and may include:
Diagnosis and monitoring
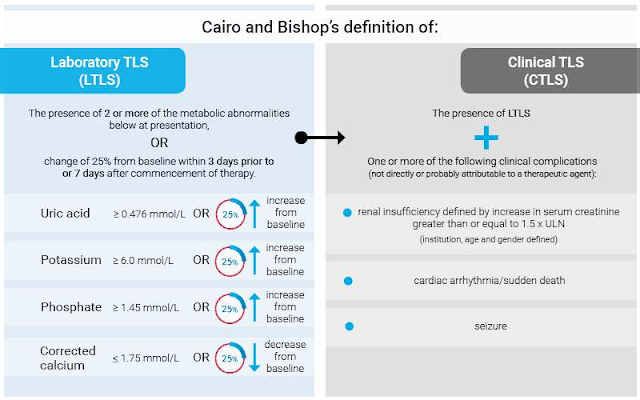
Diagnosis classifications of TLS can be divided into laboratory TLS and clinical TLS.
Blood chemistry
High-risk patients should have laboratory monitoring prior to therapy and for 48-72 hours after treatment induction. Repeat at least 3 times per day, or more often if evidence of TLS develops. Lactate dehydrogenase should be checked at least on diagnosis and prior to treatment, as elevated values can reflect the potential for progressing to TLS with the initiation of chemotherapy.
Cardiac monitoring
Frequent cardiac assessment, i.e. electrocardiography (ECG) or continuous cardiac monitoring is necessary to monitor cardiac changes or arrhythmia caused by potassium and calcium disturbances.
Imaging studies
 |
| Radiography of the chest is useful to determine the presence of a large tumour (eg. mediastinal mass). |
 |
| Perform ultrasonography or computed tomography (CT) scanning of the abdomen and retroperitoneum immediately if renal failure or mass lesions in the abdomen are present. |
 |
| Intravenous (IV) contrast may be contraindicated in a patient with renal insufficiency. |
Nursing monitoring
Treatment and management
TLS is best managed if it is anticipated and treatment is started before initiation of chemotherapy.
Treatment centres on the following:
Volume depletion is a major risk factor for TLS and must be corrected vigorously. Aggressive IV hydration not only helps to correct electrolyte disturbances by diluting extracellular fluid, it also increases intravascular volume. Increased volume enhances renal blood flow, glomerular filtration rate, and urine volume to decrease the concentration of solutes in the distal nephron and medullary microcirculation.
Hypouricaemic agents- Allopurinol
Allopurinol is a xanthine oxidase inhibitor; it is administered to reduce the conversion of nucleic acid by-products to uric acid in order to prevent urate nephropathy and subsequent oliguric renal failure.
It is usually given orally at 600 mg daily for prophylaxis and 600-900 mg daily (up to a maximum of 500 mg/m2 daily) for treatment of TLS. Patients unable to take oral medications can be given IV allopurinol.
Adverse effects may include rash, acute interstitial nephritis, pneumopathy, fever, and eosinophilia. There is a risk of acute obstructive renal failure, due to an increase of xanthine in plasma and precipitate in the renal tubules with allopurinol.
Dose reduction is necessary in renal insufficiency or if the medication is given concomitantly with cyclophosphamide, high dose methotrexate, mercaptopurine and azathioprine (since allopurinol interferes with the metabolism of these agents).
Hypouricaemic agents- Rasburicase
Rasburicase (recombinant urate oxidase) can be used when uric acid levels cannot be lowered sufficiently by standard approaches.
Rasburicase is useful in cases of hyperuricemia and has been shown to be safe and effective in both paediatric and adult patients. It also has a more rapid onset of action than allopurinol.
Humans do not express urate oxidase, which catalyses the conversion of poorly soluble uric acid to soluble allantoin. By converting uric acid to water-soluble metabolites, urate oxidase effectively decreases plasma and urinary uric acid levels.
Unlike allopurinol, uricase does not increase excretion of xanthine and other purine metabolites; therefore, it does not increase tubule crystallisation of these compounds.
HCM is primarily due to bone resorption and release of calcium in bones and is often seen in patients with multiple myeloma. Symptoms are generally non-specific including nausea and vomiting, anorexia, fatigue, bone pain and constipation, but can progress to life-threatening dehydration and altered level of consciousness.
Hypercalcaemia is a complex metabolic abnormality that affects up to 30% of people with cancer. It is characterized by high calcium levels in the blood stream.
Hypercalcaemia is a complex metabolic abnormality that affects up to 30% of people with cancer. It is characterized by high calcium levels in the blood stream.
Cancers which commonly cause hypercalcaemia include breast cancer, renal cancer, multiple myeloma, lymphoma, and squamous cell cancers. Hypercalcaemia is more common in those with advanced cancer but may also be a presenting symptom in patients with a new diagnosis.
Many cancer therapies, such as antineoplastic agents can also induce or exacerbate hypercalcaemia, particularly when used in combination.
In a healthy person, serum calcium is kept within normal levels by homeostatic mechanisms designed to balance the flow of calcium between bone, kidneys, intestines, and extracellular fluid. When serum calcium levels drop below normal, the parathyroid gland releases parathyroid hormone or PTH. PTH stimulates the release of calcium from the bones and reabsorption of calcium by the kidneys. The kidneys are also stimulated to release active vitamin D, or calcitriol. Calcitriol signals the GI tract to increase calcium absorption. These mechanisms work together in a tightly regulated and continual process to maintain calcium serum levels within a normal range.
Cancer can interrupt this regulatory process, resulting in abnormally high levels of calcium to build up in the blood. Cancers can achieve this in a number of ways, for example, some secrete a protein which mimics the action of parathyroid hormone, others secrete calcitriol and some cause increased bone destruction, all which contribute to increased serum calcium levels.
Hypercalcaemia can be mild, moderate or severe.
Left untreated severe hypercalcaemia can result in cardiac arrest, coma and death and is considered a medical emergency.
Signs and symptoms
As hypercalcaemia can affect several organ systems, initially it may be asymptomatic or present with non-specific symptoms.
The symptoms of hypercalcaemia may be similar to that of advanced malignancy and the side-effects of chemotherapy or analgesia. It is important to consider the possibility of HCM in any patient with a cancer diagnosis who presents with the following signs and symptoms.
Severity of symptoms experienced are dependent upon both the absolute calcium level as well as how quickly calcium levels have risen.
Assessment and immediate interventions
The following may be undertaken in the assessment of people with suspected hypercalcaemia.
Determine the severity and urgency of intervention required and take the appropriate action.
Moderate cases, which produce marked symptoms, and severe cases, regardless of symptoms, require prompt treatment.
Nursing interventions and support
💢Nurses have an important role to play in supporting individuals affected by hypercalcaemia, and in managing side effects.
💢Close observation is necessary in those patients suffering cardiac or central nervous system dysfunction secondary to hypercalcaemia, to prevent significant and potentially life threatening complications.
💢Patients with life threatening complications may require an ICU consult and ICU admission.
💢The patient’s Oncologist/Haematologist and treating team should be notified if a patient develops hypercalcaemia to ensure ongoing treatment, monitoring and advice.
Investigations and diagnosis
A diagnosis of hypercalcaemia is achieved by examining the total serum calcium values and adjusting for albumin concentrations to determine the patients “corrected serum calcium”. This gives an indication of the amount of ionized (active) calcium.
If serum albumin is significantly deranged, measurement of ionized calcium (if available) may be preferable.
Other diagnostic tests may include:
 |
💦 Blood sampling as clinically indicated. 💦 Serum creatinine and GFR to assess renal function 💦 Urea and electrolytes for information on metabolic/hydration status 💦 Phosphate and magnesium level 💦 Parathyroid hormone (PTH) to consider differential for etiology 💦 Parathyroid-related hormone protein (PTHrP) 💦 1,25-dihydroxy vitamin D (1,25(OH)2D) 💦 25-hydroxy vitamin D (25(OH)D) |
 |
| ECG to look for shortened QT interval or other conduction abnormalities. |
 |
Imaging with Bone Scan or PET-CT scan to identify metastatic bone disease
|
TREATMENT
The aim of treatment is to improve symptoms and reduce corrected calcium level to within the normal range and, if possible, treating the underlying disease.
Repeated blood sampling may be required for ongoing monitoring during treatment. Frequency should depend on the patient’s clinical condition and response to ongoing treatment.
Bisphosphonate therapy
Bisphosphonates bind to the bone matrix and inhibit osteoclast action and therefore bone resorption. They have no effect on the renal mechanism of hypercalcaemia.
After bisphosphonate treatment the serum calcium level will begin to fall within 12 hours and will reach the nadir within approximately four to seven days. The serum calcium level generally will remain in the normal or near-normal range for one to three weeks.
Denosumab
Denosumab is a monoclonal antibody that inhibits osteoclast activation and function. It may be an option for patients with hypercalcaemia that is refractory to zoledronic acid or in whom bisphosphonates are contraindicated due to severe renal impairment.
Regular monitoring of calcium is important as the risk of hypocalcaemia is high, particularly in patients with reduced renal function or those with insufficient vitamin D levels.
Calcitonin
Calcitonin blocks osteoclast activity and renal tubular reabsorption of calcium. The effect is rapid, usually within a few hours of first administration. Calcitonin has a limited duration of effect and is most beneficial in symptomatic patients with severe hypercalcaemia when combined with hydration and bisphosphonates. Calcitonin and hydration provide a rapid reduction in serum calcium concentration, while a bisphosphonate provides a more sustained effect.
Glucocorticoids
Corticosteroids can be given, but may only be useful where hypercalcaemia is due to:
💦 sarcoidosis
💦 lymphoma
💦 vitamin D intoxication
💦 multiple myeloma.
💦 Additionally they often take several (~ 2-4 days to achieve the desired effect).
Other treatment considerations
Discontinuing other treatments that may increase serum calcium is also necessary for effective treatment of hypercalcaemia. This may include:
💦 stopping any calcium or vitamin D supplementation
💦 thiazide diuretics
💦 lithium
Encourage patients to maintain fluid intake unless contraindicated because of a cardiac or renal conditions, and to maintain their nutritional intake.
* Alert *
Forced saline diuresis is NOT recommended as a routine treatment option. Forced saline diuresis is potentially dangerous and may cause:
💦a worsening of hypercalcaemia if dehydration is induced
💦fluid overload if insufficient diuretic is administered.
Judicious use of diuretics may be necessary to manage fluid overload in patients requiring vigorous hydration to normalize calcium levels.
DIC is a serious condition which causes both excessive blood clotting and excessive bleeding and is often seen in patients with APML.
DIC may be a chronic condition which evolves slowly, primarily causing clotting and resulting in few symptoms or it may present acutely, primarily causing bleeding and a rapid onset of symptoms. In either setting, DIC may quickly become life-threatening and is considered an oncological emergency.
Normally, when there is an injury to a blood vessel, the vessel constricts to reduce blood loss. Circulating platelets become activated, they swell and stick together to form a loose platelet plug over the injured area.
Clotting and coagulation factors circulating the blood stream are also activated, this is called activation of the clotting cascade which leads to the production of fibrin. Fibrin becomes enmeshed in the platelet plug to form a stable clot.
Some cancers, such as gastric, pancreatic, ovarian and some leukaemias may produce large amounts of pro-coagulants. These pro-coagulants activate the clotting cascade unnecessarily, resulting in multiple blood clots to form in blood vessels throughout the body. These bloods clots can damage internal organs such as the kidneys, liver, spleen and lungs.
This excessive clotting also depletes the levels of coagulation proteins and platelets in the blood, reducing the body’s ability to form further clots. This results in excessive bleeding.
DIC will not resolve unless the underlying cause is treated. Left untreated, DIC can lead to multiple organ failure and death and is considered and oncological emergency.
Acute DIC relating to oncological emergencies may also be caused by:
💦 Severe sepsis
💦 Transfusion and immunological reaction
Signs and symptoms
The symptoms of Disseminated Intravascular Coagulopathy (DIC) may develop quickly over hours or days, or more slowly. It is important that all health professionals feel confident in recognizing the signs and symptoms of DIC, assessing severity and escalating care appropriately.
Signs and symptoms associated with DIC include:
Assessment and initial management
If you recognize the signs and symptoms of acute DIC in a patient, take action
Immediate nursing interventions
Investigations and diagnosis
A diagnosis of DIC is made on clinical and laboratory findings.
No single laboratory test can accurately confirm or eliminate the diagnosis.
A full medical history and clinical examination should be performed to:
💦 identify any underlying cause for the DIC
💦 identify any potential thrombotic or hemorrhagic consequences.
Blood laboratory investigations should include:
💦 full blood count including platelet count,
💦 coagulation studies including prothrombin time (PT-INR) activated partial thromboplastin time (aPTT), D-dimer and fibrinogen level
💦other as clinically indicated to investigate the underlying cause.
Pathology
To assist in diagnosis of DIC, the International Society on Thrombosis and Haemostasis (ISTH) provide a scoring system.
Using the scoring system, DIC may be diagnosed if a patient is affected by an underlying disorder known to be DIC-related has a total score ≥5.
If the score is <5, laboratory tests should be repeated. However, the laboratory tests used to diagnose DIC require an understanding of the underlying disease and the patients clinical status
Treatment and management
DIC will not improve until the underlying cause or trigger is treated. Do not delay treatment, support coagulation and vital organ function.
The treatment of DIC is dependent upon pathology, severity and patient treatment goals. The main goals of treatment for DIC are to control clotting and bleeding and correct the underlying cause.
Key elements
In the presence of widespread bleeding, replacement with blood component therapy is recommended.
There are four different blood products that can be given to help return blood levels to normal.
The following is a summary of the Australian Red Cross Blood Service (2014) Management of DIC recommendations.
Initiate serial blood testing to determine if coagulation and fibrinolysis are worsening or improving.
The frequency of testing depends on the severity of clinical findings and management. Daily, twice-daily, or even more frequent testing may be appropriate in an acutely ill patient with active bleeding or thrombosis.
Resolution of DIC
DIC does not resolve immediately once the underlying factor is corrected. Resolution generally requires:
💦 blood coagulation factors returning to normal levels
💦 clearance of clotting factor and fibrin break down products from the circulation
💦 production of new platelets which may take several days.
DIC will usually begin to improve within a few days after the trigger is removed or terminated. Underlying organ damage may extend the rate of improvement.
Mediastinal tumours and enlarged mediastinal lymph nodes may compress or obstruct the superior vena cava, a vein which carries blood from the upper body to the heart.
Superior vena cava obstruction (SVCO) can result in death and is considered an oncological emergency.
The symptoms of SVCO result from increased venous pressure caused by a back-up of blood in the veins of the upper body.
The veins in the neck and chest dilate, fluid is forced into surrounding tissues resulting in swelling of the face, neck and arms and increased pressure on the trachea leading to breathing difficulties.
The superior vena cava or SVC is a vein located in the right side of the chest. It carries blood from the head, neck, upper limbs and upper thorax back to the heart.
Tumours and enlarged mediastinal lymph nodes can compress or directly invade the SVC, blocking the return of blood flow from the upper body back to the heart. This is called an SVC obstruction or SVCO.
The symptoms of SVCO result from increased venous pressure caused by a back up of blood in the veins of the upper body. The veins in the neck and chest dilate, fluid is forced into surrounding tissues resulting in swelling of the face, neck and arms and increased pressure on the trachea leading to breathing difficulties.
SVCO is a medical emergency. Left untreated it can result in breathing compromise, cerebral edema and death.
Signs and symptoms
The symptoms of superior vena cava syndrome (SVCS) can vary from mild to life threatening according to the degree of obstruction. It is important that all health professionals feel confident in recognizing the signs and symptoms of SVCS, assessing severity and escalating care appropriately.
Signs and symptoms associated with SVCS include:
💦 Headaches
💦 confusion, dizziness
💦 syncope
💦 chest pain
💦 stridor (due to laryngeal oedema)
💦 dyspnea
💦 dysphagia
💦 cough
💦 dilated chest veins
💦 swelling of the neck and upper extremities
💦 facial plethora (typically described as being worse in the morning)
💦 haemoptysis
💦Pemberton’s sign (Patients with SVC obstruction will often become plethoric and/or breathless when both arms are raised above their head for over 60 seconds).
💦 cyanosis (blue or grey tinge to the skin)
💦 hoarseness
 |
| Positive Pemberton’s sign: bilateral arm elevation causes facial plethora. |
 |
Patient with SVCO demonstrating facial plethora and neck swelling
|
Assessment and initial management
If you recognize the signs and symptoms of SVCO in a patient, take action without delay.
Assess airways, breathing and circulation.
Take a thorough clinical history:
💦 assess history of malignancy
💦 record previous and current treatments
💦 assess the severity, duration and speed of onset of symptoms.
These are important in determining the urgency of intervention.
Grading and interventions
Determine the grade and urgency of intervention required.
Take the appropriate action.
Immediate nursing interventions
Investigations and diagnosis
Imaging
Patients may receive the following as a part of the diagnostic work-up for SVCO.
💦 Chest X-Ray
 |
| Chest X-ray (CXR) |
Often abnormal in SVCO
Can identify mediastinal masses, pleural effusions, lobar collapse or a mediastinal widening
💦Chest Computed tomography (CT) or Magnetic Resonance Imaging (MRI)
👉 Gold standard investigation
👉Useful in assessing site, pathology, tumour/mass size, SVC diameter, length of obstruction and evidence of thrombus
👉 May be used to guide biopsy attempts
Pathological diagnosis
Treatment of SVCO is determined by the underlying pathology. Patients may have a biopsy to confirm diagnosis.
Treatment
There are numerous treatment options for SVCO. Appropriate treatment options are determined by the underlying pathology.
Learn about the different treatment options for SVCO management and the health professionals involved so that you can prepare and inform your patients about their care.
Multidisciplinary team
Corticosteroids such as dexamethasone are sometimes used as an initial intervention to reduce the pressure and swelling around the blood vessel and improve symptoms such as breathlessness.
Radiotherapy
The majority of the tumour types causing SVCO are sensitive to radiotherapy.
Often used as the primary intervention or after stenting.
Effective for symptoms relief, 75% of patients with malignancy-associated SVCO experience improvement within 3–7 days.
For some malignancies, chemotherapy is given concurrently with radiation.
Chemotherapy
Chemotherapy works effectively for chemotherapy sensitive cancers (e.g. small cell lung cancer, germ cell tumours and non-Hodgkin’s lymphoma).
Surgery
Surgery may be considered to bypass or resect tumours in order to decompress the SVC.
The role of surgery is limited in this palliative setting. However, may be effective in select patients with a good prognosis who are medically and surgically operable.
Stent placement
An intravascular stent is placed to bypass the obstruction of the SVC.
Considered for patients with severe symptoms that require urgent intervention or whose treatment options are limited.
Effective for symptom relief, 97–99% of patients experiencing rapid post-operative relief
* Alert *
Medical treatment is dependent upon pathology, severity and patient treatment goals. Treatment modalities can be used alone or in combination. Management is at the discretion of the treating team in accordance with local procedures and policies.
Keep these 3 simple tips in mind when educating patients:
💦Practice universal health literacy precautions - Assume all patients are at risk for having difficulty comprehending health information.
💦 Personalize information – Identify individual patient education needs and tailor information to match.
💦 Practice the teach back method - Ask patients to explain back the information you have given.
Let’s look at some examples of delivering patient information, but first let’s meet Jane.
Example 1
Although Jane's nurse in Example 1 technically did her job instructing Jane about her new medication, she assumed that Jane would understand medical terms such as ‘neutropenia’ and the abbreviation ‘subcut’.
She ignored the possibility that a physiotherapist may have no experience with chemotherapy and specific drug administration.
In Example 2, the nurse recognized that despite Jane’s clinical background, she may still have difficulty comprehending health information.
By using simple language and avoiding medical jargon, Jane's nurse in Example B has made it really easy for Jane to understand why and how she should take the medication.
Tip 1: Practice universal health literacy precautions
Assume all patients are at risk for having difficulty comprehending health information.
Example A
Example B
You can see the differences in these two examples, Jane's nurse in Example A did not reinforce messages with written materials and did not personalize any information for Jane. She assumed that Jane is familiar with medication labels, knows the hospital system and how to get help and will be able to recognize situations that require urgent care, such as identifying the signs and symptoms of febrile neutropenia.
In Example B, Jane’s nurse personalized written materials by crossing out irrelevant information and highlighting important and essential points. She also included extra information such as phone numbers, etc.
Tip 2: Personalize information
Identify individual patient education needs and tailor information to match.
Example C
Jane's nurse in Example C asked closed questions rather than using the teach-back method and did not confirm that Jane had correctly interpreted the information.
Jane may be highly stressed and anxious, rendering her unable to focus on learning.
In Example D, Jane's nurse created a respectful and shame free learning environment by asking open-ended questions and reinforcing key messages until Jane fully understood her medication.
This involved clarifying information, reinforcing key messages, and repeating this process until Jane was able to ‘teach back’ the information successfully. A blame-free environment was created by taking responsibility for any miscomprehension and offering alternative explanations.
Tip 3: Practice the teach back method
Ask patients to explain back the information you have given.












































































Comments
Post a Comment