 |
| | HAEMATOLOGICAL DISEASES & DISORDERS |
|
LEARNING OBJECTIVES:
At Completion of this module you will be able to:
🌸differentiate between malignant & non malignant haematological diseases
🌸describe the key clinical features of leukemia, lymphoma and myeloma
HAEMATOLOGY
Hematology relates to the management of blood disorders and blood cancers; they are divided into two categories:
Malignant and Non Malignant Diseases.
Non-malignant haematological diseases
- Group of non- cancer blood disorders.
- They can be autoimmune or inherited and some may be pre-malignant
- They have the potential to transform into cancer in the future.
- This includes some of the myelodysplastic and myeloproliferative disorders.
Malignant Hematological diseases: is the uncontrolled proliferation of blood cells throughout their development , there are three major classifications of malignant hematological diseases.
RISK FACTORS LINKED TO AN INCREASE RISK OF HAEMATOLOGICAL CANCER
TYPES OF BLOOD CANCER
LEUKEMIA
Leukemia is a disorder of the leucocytes, characterized
by the uncontrolled proliferation of abnormal cells.
This leads to overcrowding of the bone marrow, so that
healthy cells are unable to replicate, mature and carry
out normal functions in the blood.
Leukemia is a cancer of the cells in the bone marrow and blood. It usually begins as an uncontrolled growth of abnormal leucocytes in the bone marrow which do not mature or function properly. This leads to the bone marrow becoming overcrowded with non-functioning cells, leaving no room for healthy cells to mature and carry out normal functions. Leukaemia can be either acute or chronic and arise in either the lymphoid or myeloid stem cell lineage. Acute leukaemia usually involves the overproduction of immature leucocytes or blast cells and can advance rapidly. Chronic leukaemia typically involves the overproduction of mature leucocytes and as the name suggests advances slowly.
Acute and Chronic Leukemia:
Acute leukemia involves the rapid proliferation of immature leukocytes also called blast cells.
Acute leukemia can arise on the myeloid stem cell lineage (Acute Myeloid Leukemia-AML) and (Acute Promyelocytic Leukemia -APML) or the lymphoid stem cell lineage (Acute Lymphocytic / Lymphoblastic leukemia)
Acute Myeloid Leukemia
Acute myeloid leukemia (AML) is a type of blood cancer. It starts in your bone marrow, the soft inner parts of bones. AML usually begins in cells that turn into white blood cells, but it can start in other blood-forming cells.

Risk Factors :
✔ Elderly age
✔ Gender: Higher in male
✔ Smoking
✔ Exposure to certain chemicals
✔ History of treatment with chemotherapy drugs
✔ Radiation exposure
✔Blood disorders such as polycythemia vera, thrombocythemia, and idiopathic myelofibrosis
✔ Genetic disorders such as
- Fanconi anemia
- Bloom syndrome
- Ataxia-telangiectasia
- Diamond-Blackfan anemia
- Shwachman-Diamond syndrome
- Li-Fraumeni syndrome
- Severe congenital neutropenia (also called Kostmann syndrome)
- Down syndrome
- Trisomy 8
✔ Family History
Signs and Symptoms :
General symptoms:
Symptoms from low red blood cell counts:
👉Tiredness
👉Weakness
👉Dizziness
👉Headache
👉Pale Skin
👉Shortness of breath
Symptoms from low white blood cell counts:
📌Neutropenia
📌Recurrent Infections
📌Fever
Symptoms from low blood platelet counts:
🔔 Bruises
🔔 Frequent or severe nosebleeds
🔔 Frequent or severe nosebleeds
🔔 Bleeding gums
🔔 Heavy menstrual bleeding in women
Symptoms from high numbers of leukemia cells:
The cancer cells in AML (called blasts) are bigger than normal white blood cells and have more trouble going through tiny blood vessels.
If the blast count gets very high, these cells can clog up blood vessels and make it hard for normal red blood cells (and oxygen) to get to tissues, this is called leukostasis.
Some of the symptoms are like:
🍡 Headache
🍡 Weakness in one side of the body
🍡 Slurred speech
🍡 Confusion
🍡 Sleepiness
When blood vessels in the lungs are affected, people can have shortness of breath. Blood vessels in the eye can be affected as well, leading to blurry vision or even loss of vision.
Other Symptoms include:
☄ Bone or Joint pain
☄ Deep Vein Thrombosis
☄ Pulmonary embolism
☄ Swelling in the abdomen
Acute Promyelocytic Leukemia
Acute promyelocytic leukemia (APL) is a blood cancer characterized by a marked increase in a type of white blood cells known as promyelocytes, a type of immature white blood cell.
Prompt diagnosis and treatment of acute promyelocytic leukemia (APL), the M3 subtype of acute myeloid leukemia (AML), is very important because patients with APL can quickly develop life-threatening blood-clotting or bleeding problems if not treated.
Acute lymphocytic leukemia (ALL)
Acute lymphocytic leukemia (ALL) is a type of cancer of the blood and bone marrow — the spongy tissue inside bones where blood cells are made
The word "acute" in acute lymphocytic leukemia comes from the fact that the disease progresses rapidly and creates immature blood cells, rather than mature ones.
Signs and Symptoms :
🌂Bleeding from the gums
🌂Bone pain
🌂Fever
🌂Frequent infections
🌂Frequent or severe nosebleeds
🌂Lumps caused by swollen lymph nodes in and around the neck, armpits, abdomen or groin
🌂Pale skin
🌂Shortness of breath
🌂Weakness, fatigue or a general decrease in energy
Risk Factors :
Factors that may increase the risk of acute lymphocytic leukemia include:
1. Previous cancer treatment:
Children and adults who've had certain types of chemotherapy and radiation therapy for other kinds of cancer may have an increased risk of developing acute lymphocytic leukemia.
2.Exposure to radiation:
People exposed to very high levels of radiation, such as survivors of a nuclear reactor accident, have an increased risk of developing acute lymphocytic leukemia.
3. Genetic disorders:
Certain genetic disorders, such as Down syndrome, are associated with an increased risk of acute lymphocytic leukemia.
Chronic Leukemia involves the overproduction of mature abnormal leucocytes. Chronic leukemia typically progresses more slowly than acute leukemia.
- Patients commonly present without symptoms, and the disease is often discovered when a routine blood test shows a high leucocyte count.
- Chronic leukemia can also arise on the myeloid stem cell lineage (chronic myeloid leukemia (CML)or the lymphoid stem cell lineage(Chronic Lymphocytic leukemia)
Chronic Myeloid Leukaemia
Chronic myelogenous (myeloid) leukemia(CML) is an uncommon type of cancer of the bone marrow — the spongy tissue inside bones where blood cells are made. CML causes an increased number of white blood cells in the blood.
CML is described in three phases:
1. Chronic - a few blast cells (immature leucocytes) are found in the blood and bone marrow.
2. Accelerated - after a few years , the leukemia suddenly changes and cell growth accelerates.
3. Blast Crisis - the number of blast cells(immature leucocytes) increase causing symptoms to worsen. Blast cells often spread to other organs.
Signs and Symptoms :
👉Bone pain
👉Easy bleeding
👉Feeling full after eating a small amount of food
👉Feeling run-down or tired
👉Fever
👉Weight loss without trying
👉Loss of appetite
👉Pain or fullness below the ribs on the left side
👉Excessive sweating during sleep (night sweats)
Risk Factors :
💢Older age
💢Being male
💢Radiation exposure
Chronic Lymphocytic Leukaemia
Chronic lymphocytic leukemia (CLL) is a type of cancer of the blood and bone marrow — the spongy tissue inside bones where blood cells are made.
The term "lymphocytic" in chronic lymphocytic leukemia comes from the cells affected by the disease — a group of white blood cells called lymphocytes, which help your body fight infection.
Chronic lymphocytic leukemia most commonly affects older adults. There are treatments to help control the disease.
BINET system for staging CLL:
Signs & Symptoms :
👉Bruising and unusual bleeding caused by a low platelet count
👉Repeated infections -caused by a low white blood cell count
👉 Swollen lymph nodes/ spleen
👉 Bone pain or tenderness
👉 Frequent or severe infection
Risk Factors :
Complications
🏁Frequent infections
🏁A switch to a more aggressive form of cancer
🏁Increased risk of other cancer
🏁Immune system problems
How is leukemia diagnosed?
💧 Complete Blood Count
💧 Bone marrow analysis
💧 Imaging studies : X-ray, CT Scan, MRI, Ultrasound Scan, PET Scan
💧 Lumbar Puncture
💧 Cell Assessment for gene or chromosome changes
💧 Physical examination
Treatments for Leukemia
Common treatments often include a combination of the following:
1. Chemotherapy:
Chemotherapy is the most common form of leukemia treatment. It involves using chemo drugs to destroy leukemia cells or keep them from multiplying.
Phases of Chemotherapy in AML
Induction Therapy:
💫The goals of induction therapy are to destroy as many cancerous cells as possible, restore healthy blood cell counts to normal levels and induce remission so that no evidence of cancer remains .
💫Many patients receive a combination of anthracycline, doxorubicin and cytarabine, which is administered intravenously in several sessions over the course of four to six weeks. Some patients receive several rounds of induction therapy before reaching remission.
Post remission Therapy:
💫Used for reducing the likelihood of recurrence by destroying residual cancer cells that went undetected in blood and bone marrow tests.
💫The treatment usually consists of four cycles of intensive chemotherapy that includes high doses of cytarabine and one or more other drugs
Maintenance Therapy:
💫Patients with certain types of AML receive maintenance treatment consisting of low doses of chemotherapy administered over the course of several months or years
Phases of Chemotherapy in ALL
Induction Therapy:
💫Induction regimens for ALL generally use a combination of drugs that include:
- Vincristine
- Anthracyclines (daunorubicin , doxorubicin )
- Corticosteroids (prednisone, dexamethasone)
- With or without asparaginase and/or cyclophosphamide
- At the end of induction therapy, doctors will check to see whether the patient has achieved a complete remission.
A complete remission is achieved when
- No more than 5 percent of cells in the bone marrow are blast cells
- Blood cell counts are back to normal
- All signs and symptoms of ALL are gone.
Consolidation Therapy:
💫The second phase of chemotherapy is called “consolidation” therapy or "intensification" therapy. During this phase, the chemotherapy drugs are given in higher doses than those given during the induction phase.
💫The combination of drugs and the duration of therapy for consolidation regimens vary but can consist of combinations of drugs similar to those drugs used during the induction phase.
💫Several chemotherapy drugs are combined to help prevent the leukemia cells from developing drug resistance.
💫Some of the drugs used in the consolidation treatment phase include
- High-dose methotrexate
- Cytarabine
- Vincristine
- 6-mercaptopurine (6-MP)
- Cyclophosphamide
- Pegaspargase
- Corticosteroids (prednisone, dexamethasone)
Maintenance Therapy:
💫The third phase of ALL treatment is called “maintenance.” The goal of maintenance therapy is to prevent disease relapse after induction and consolidation therapy.
💫Most maintenance drugs are given orally and, typically, patients are treated in an outpatient setting.
They receive lower doses of chemotherapy drugs and, as a result, tend to have less severe side effects.
💫In some cases, post remission chemotherapy also includes drugs that were not used during induction treatment.
💫Most maintenance regimens include
- 6-mercaptopurine (administered daily)
- Methotrexate (administered weekly)
- Periodic doses of vincristine and corticosteroids
Central nervous system-directed therapy may include:
Intrathecal chemotherapy: Anticancer drugs are injected into the fluid-filled space between the thin layers of tissue that cover the brain and spinal cord. These drugs may include methotrexate, cytarabine and corticosteroids (prednisone, dexamethasone).
High-dose systemic chemotherapy : Anticancer drugs travel through the blood to cells all over the body. These drugs may include high-dose methotrexate, intermediate-/high-dose cytarabine and pegaspargase.
Cranial irradiation: Radiation therapy to the brain.
Chemotherapy in CLL
Standard chemotherapy drugs that are used to treat CLL as a single agent or in combination include:
Antimetabolites
- Cladribine
- Fludarabine
- Pentostatin
Alkylating agents
- Bendamustine hydrochloride
- Chlorambucil
DNA-Damaging Agent
Corticosteroids
2. Immunotherapy: This treatment uses certain drugs to boost body’s defense system - immune system to fight leukemia. Immunotherapy helps your immune system identify cancer cells and produce more immune cells to fight them
3. Stem cell transplant : may be an option for some people younger than 55 years of age.
4.Radiation therapy: is most often used to prevent leukemia from spreading to, or treat leukemia that has spread to, the central nervous system (CNS). It is also used to prepare the bone marrow for stem cell transplant.
5. Targeted therapy:
This treatment uses drugs designed to attack specific parts of a leukemia cell (like a protein or gene) that are causing them to overtake normal blood cells. Targeted therapies may prevent leukemia cells from multiplying, cut off the cells’ blood supply or kill them directly. Targeted therapy is less likely to harm normal cells. Examples of targeted therapy drugs include monoclonal antibodies and tyrosine kinase inhibitors.
6. Supportive therapy : is given to manage the expected complications of the leukemia and its treatments.
7. Hematopoietic cell transplant (stem cell or bone marrow transplant):
This treatment replaces the cancerous blood-forming cells killed by chemotherapy and/or radiation therapy with new, healthy hematopoietic cells
LYMPHOMA
Lymphoma is a diverse group of cancers that arise in the lymphatic system when normal lymphocytes undergo malignant changes during the maturation process, becoming lymphoma cells.
Lymphoma is a group of cancers that occur when normal lymphocytes undergo malignant changes and become lymphoma cells. These lymphoma cells grow and multiply, forming tumors that can occur in the lymphatic system and other places in the body, such as the liver, spleen, stomach and central nervous system.
Lymphoma is broadly classified into two groups: Hodgkin lymphoma and Non-Hodgkin lymphoma. Hodgkin lymphoma can be distinguished from other types of lymphoma by the presence of an abnormal cell called the Reed-Sternberg cell. This is usually found via a lymph node biopsy. Non-Hodgkin lymphoma is a group of diseases, classified by the type of lymphocyte from which they originally develop, i.e a B-cell or T-cell lymphoma
Lymphoma is classified into two groups:
✒ Hodgkin lymphoma
✒ Non-Hodgkin lymphoma
Hodgkin lymphoma
Hodgkin lymphoma is distinguished from all other types of lymphoma by the presence of an abnormal cell called the Reed-Sternberg cell
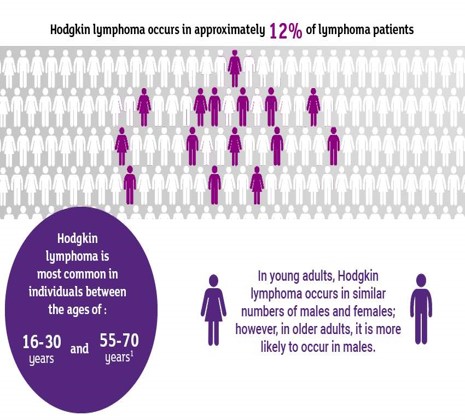
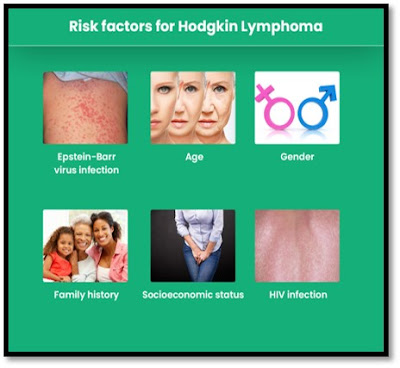
Risk Factors :
📏Epstein -Barr Virus Infection
📏Age:
People can be diagnosed with HL at any age, but it's most common in early adulthood (especially in a person’s 20s) and in late adulthood (after age 55)
📏Gender:
HL occurs slightly more often in males than in females.
📏Family history:
Brothers and sisters of young people with this disease have a higher risk for HL. The risk is very high for an identical twin of a person with HL.
📏Weakened immune system:
The risk of HL is increased in people infected with HIV, the virus that causes AIDS.
Signs and Symptoms :
The most common symptom of Hodgkin lymphoma is one or more enlarged (swollen) lymph nodes. The enlarged lymph node may be in the neck, upper chest, armpit, abdomen or groin. The swollen lymph node is usually painless.
General Symptoms:
📍Painless swelling of lymph nodes in your neck, armpits or groin
📍High temperatures that come and go with no obvious cause, often overnight
📍Losing a lot of weight over a short period of time, despite eating well
📍 Itching, which may be worse after drinking alcohol
cough or shortness of breath
Hodgkin lymphoma in the bone marrow:
📍Shortness of breath and tiredness because of anemia from a low red blood cell count
📍Increased risk of infections because of a low white cell count
📍Bleeding problems such as nosebleeds, very heavy periods, or a rash of tiny blood spots under the skin because of a low platelet count
Other possible symptoms:
📍Pressure on nerve which cause pain
📍swelling in arms or legs by blocking the flow of lymphatic fluid around the body
📍 Jaundice caused by blocking of bile flow from liver.
Diagnosis :
The World Health Organization (WHO) divides Hodgkin lymphoma into two main subtypes. They are:
📛 Classical Hodgkin lymphoma
📛 Nodular lymphocyte-predominant Hodgkin lymphoma
Classical Hodgkin lymphoma is characterized by the presence of both Hodgkin and Reed-Sternberg cells.
Nodular lymphocyte-predominant Hodgkin lymphoma is characterized by the presence of lymphocyte-predominant cells, sometimes termed “popcorn cells,” which are a variant of Reed-Sternberg cells.
🔌Most common in 30 to 50 year-old age group
🔌More common in males
🔌Slow growing and can relapse many years later
🔌Highly curable
🔌Small risk of transformation to aggressive non-Hodgkin lymphoma
Staging :
Lymphoma is graded, based on how aggressive the disease is i.e. how fast it grows and spreads throughout the body and it needs to be treated.
The staging of lymphoma is determined using several tests, including

The current recommended staging system is known as the Lugano staging system , this was adapted from the Ann Arbor Staging System and includes Cotswolds modifications for Hodgkin Lymphoma.
The Lugano staging system as below:

Treatment:
The goal of Hodgkin's lymphoma treatment is to destroy as many of the lymphoma cells as possible and bring the disease into remission.
Chemotherapy:
Classical Hodgkin's lymphoma treatment usually begins with chemotherapy. It may be the only treatment needed or it may be combined with radiation therapy.
For nodular lymphocyte-predominant Hodgkin's lymphoma, chemotherapy is often combined with drugs that target the cancer cells (targeted therapy) and radiation therapy.
Radiation therapy:
Hodgkin's lymphoma treatment, radiation can be aimed at affected lymph nodes and the nearby areas where the disease might spread. It's usually used with chemotherapy. For people with early-stage nodular lymphocyte-predominant Hodgkin's lymphoma, radiation therapy may be the only treatment needed.
Bone marrow transplant:
A bone marrow transplant may be an option if Hodgkin's lymphoma returns or doesn't respond to other treatments.
Other drugs that are sometimes used to treat Hodgkin's lymphoma include:
Targeted therapy: Targeted drug treatments focus on specific weaknesses present within cancer cells. By blocking these weaknesses, targeted drug treatments can cause cancer cells to die.
Immunotherapy: For Hodgkin's lymphoma, immunotherapy might be considered in certain situations, such as if the disease doesn't respond to other treatments.
Nursing Management:
☺ Monitoring Vitals
☺Educate the patient about the disease
☺Weigh patient
☺Encourage nutrition
☺Monitor breathing and oxygen saturation
☺Not changes in color
☺Monitor for respiratory distress
☺Manage pain
☺Provide comfort measures
☺Prevent skin breakdown
Non-Hodgkin lymphoma:
Within non-Hodgkin lymphoma, there are over 80 subtypes of lymphoma.
The onset of NHL occurs most frequently in individuals over the age of 50 years. NHL is grouped according to the type of lymphocyte from which the originally develop, i.e. B-cell or T-cell lymphoma.
- 💥 Follicular Lymphoma
- 💥 Diffuse large B-cell Lymphoma
- 💥 Small Lymphocytic Lymphoma
- 💥 Mantle Cell Lymphoma
- 💥 Burkitt lymphoma
- 💥 Marginal zone Lymphoma
T- Cell Lymphomas :
💠Peripheral T-cell Lymphoma
💠Precursor T-lymphoblastic Lymphoma
💠Cutaneous T-cell Lymphoma
💠Anaplastic T-cell Lymphoma
Signs & Symptoms :
🔖Swelling in the lymph nodes in the neck, underarm, groin, or stomach.
🔖Fever of unknown reason
🔖Drenching night sweats.
🔖Weight loss
🔖Fatigue
🔖Skin rashes
🔖Pain in the abdomen
Diagnosis :

Treatment:
Treatment approaches for NHL depend on the type of cancer.
Chemotherapy:
The most common therapy for non-Hodgkin's lymphoma is called R-CHOP and consists of four different chemotherapy medications plus a type of immunotherapy called rituximab, which specifically targets some lymphoma cells. The medications are given through an IV and by mouth for five consecutive days. This is then repeated every three weeks for six to eight cycles.
Radiation therapy:
For certain types of non-Hodgkin's lymphoma, radiation therapy may be the only treatment needed. particularly if your lymphoma is slow growing and located in just one or two spots. More commonly, radiation is used after chemotherapy to kill any lymphoma cells that might remain. Radiation can be aimed at affected lymph nodes and the nearby area of nodes where the disease might progress.
Targeted drug therapy:
Targeted drug treatments focus on specific abnormalities present within cancer cells. By blocking these abnormalities, targeted drug treatments can cause cancer cells to die.
For non-Hodgkin's lymphoma, targeted drugs can be used alone, but are often combined with chemotherapy. This combination can be used as your initial treatment and as a second treatment if your lymphoma comes back.
Engineering immune cells to fight lymphoma:
CAR-T cell therapy might be an option for certain types of B-cell non-Hodgkin's lymphoma that haven't responded to other treatments.
Biological Therapy:
Biological therapy, also called immunotherapy, is a form of treatment that uses the body's immune system, either directly or indirectly, to fight cancer or to lessen the side effects that can be caused by some cancer treatments. It uses materials made by the body or in a laboratory to boost, direct or restore the body's natural defenses against disease.
The drug rituximab is an example of one type of immunotherapy that is widely used.
Stem Cell Transplant:
Stem cell transplantation, also called bone marrow transplantation, is offered to all patients with recurrent non-Hodgkin's lymphoma.
Nursing Management:
✏ Head to Toe Assessment and Focused Assessment
✏ Adequate management of symptoms and side effects related to treatment
✏ Adequate pain management
✏ Psychosocial support and coping mechanisms
✏ Decrease risk of infection
✏ Meeting patient and family goals
✏ Palliative Care
✏ Effective patient education
MYELOMA
Myeloma is a type of blood cancer that develops from plasma cells in the bone marrow. Myeloma is often called multiple myeloma because most of the people (90%) have multiple bone lesions at the time of diagnosis.
Multiple myeloma also called myeloma is a cancer of the plasma cells and occurs when abnormal plasma cells multiply uncontrollably. While healthy plasma cells produce protective immunoglobulins or antibodies, a critical part of the immune response, abnormal plasma cells produce an antibody called paraprotein, or M Protein. Paraprotein has no useful function and its increased levels in the blood or urine are considered a diagnostic indicator of myeloma and a way to monitor the disease.
The abnormal plasma cells invade the bone marrow, releasing a chemical that causes other cells to remove calcium from the bones. This can lead to pathological fractures, vertebral collapse, pain and hypercalcemia.
A high level of circulating plasma cells can also damage the kidneys and lead to renal impairment which is suggestive of poorer outcomes for myeloma patients.
Signs and Symptoms :
- Bone pain or a broken bone without an obvious injury
- Frequent infections or an infection that is difficult to overcome
- Tiredness, shortness of breath or a racing heart
- Kidney problems
- Heavy nosebleeds or easy bruising
- Feeling sick, drowsy or confused
- Abnormal blood counts
- Other Plasma Cell Disorders such as Monoclonal gammopathy
Bone marrow infiltration with myeloma cells causes anemia, thrombocytopenia and neutropenia. An abnormally high level of myeloma cells in the bloodstream can cause renal impairment or failure. Renal impairment tends to suggest a poorer prognosis for people with myeloma
Risk Factors :
Myeloma usually occurs in individuals over the age of 60 and is more common in men
Diagnosis :
💉Blood counts
💉Blood chemistry studies: Creatinine levels, Albumin, Calcium
💉Urine tests for myeloma protein
💉Quantitative immunoglobulins
💉Electrophoresis
💉Bone marrow biopsy, Fine needle aspiration biopsy, Core needle biopsy
💉Imaging studies : CT Scan, Bone x-rays, PET scan, MRI, Echocardiogram
Myeloma and Bone Pain:
💥Abnormal plasma cells (myeloma cells) produce an antibody called paraprotein (or M Protein).
💥Paraprotein has no useful function and its increased levels in the blood or urine are considered a diagnostic indicator of myeloma or a way to monitor the disease.
💥The proliferating abnormal plasma cells collect and invade the bone and bone marrow, releasing chemicals that cause osteoclasts (cells of the bone marrow) to remove calcium from the bones.
Bone pain is the most common presenting feature of myeloma, and the destruction of bone is responsible for some of the more debilitating symptoms of this disease. Pathological fractures, vertebral collapse, pain and hypercalcemia and are all related to this process.
Staging:
The most commonly used staging system for myeloma is the Revised International Staging System.
The R-ISS divides myeloma into stages I, II and III based on the results of various blood tests that check
🩸 Levels of beta-2 microglobulin (ß2M) – a protein
produced by myeloma cells that indicates the extent of disease
🩸 Levels of albumin – a protein produced by the liver
that indicates overall health
🩸levels of lactate dehydrogenase (LDH) – an enzyme
released into the blood when cells are damaged or destroyed
🩸Genetic information – the presence of one or more specific chromosomal abnormalities may identify people at highest risk of the disease progressing
Treatment:
Symptom control and preventing potential complications of myeloma are key priorities in caring for myeloma.
The CRAB criteria is often used to identify whether a person has active myeloma, which may require treatment.
Active monitoring:
Active monitoring, which involves regular check-ups, is most often used for early-stage myeloma, when it is considered that immediate treatment will not affect prognosis.
Treatments to control myeloma
Initial treatment usually includes a combination of chemotherapy and other drugs such as thalidomide and steroid.
Chemotherapy:
Chemo drugs that can be used to treat multiple myeloma include:
- Cyclophosphamide
- Etoposide
- Doxorubicin
- Liposomal doxorubicin
- Melphalan
- Bendamustine
Corticosteroids:
Corticosteroids, such as dexamethasone and prednisone, are an important part of the treatment of multiple myeloma.
They can be used alone or combined with other drugs as a part of treatment. Corticosteroids are also used to help decrease chemotherapy induced nausea and vomiting.
Immunomodulating agents:
💊Thalidomide
💊Lenalidomide
💊Pomalidomide
Radiation therapy:
If myeloma severely weakens the vertebral bones, these bones can collapse and put pressure on the spinal cord and spinal nerves. Symptoms include a sudden change in sensation ( numbness or tingling), sudden weakness of leg muscles, or sudden problems with urination or moving the bowels.
The type of radiation therapy most often used to treat multiple myeloma or solitary plasmacytoma is called external beam radiation therapy.
Stem cell Transplant
CAR- T Therapy
Supportive Treatment
Monoclonal Gammopathy of Undetermined Significance
Monoclonal gammopathy of unknown significance (MGUS) is characterized by the presence of an abnormal protein in the blood that is produced by plasma cells. Plasma cells are cells in the bone marrow that normally produce antibodies to fight infection.
The abnormal protein produced by the MGUS plasma cells is called either an M–protein or paraprotein. This abnormal protein is found in the blood and is monoclonal. Monoclonal means that it is being produced by one family of cells that are all identical copies of each other.
MGUS can be referred to as a benign condition as there is only a small risk that MGUS can develop into myeloma or a related blood disorder. The average risk of progression to active myeloma is about 1% per year.
Risk factors:
Age
MGUS is more common in older people. It is rare in people under the age of 40.
Gender
MGUS is almost twice as common in men than in women.
Family history
Siblings of patient with MGUS have a slightly increased risk of developing it.
Clinical Features:
People with monoclonal gammopathy generally don't experience signs or symptoms. Some people may experience rash or nerve problems, such as numbness or tingling.
Treatment and monitoring:
💊MGUS does not require any active treatment, however monitoring is recommended.
💊Monitoring of MGUS includes regular clinical assessment and follow up measurements of serum protein.
💊The serum protein should be checked after three months and then again at six months to establish a firm diagnosis of MGUS.
Myelodysplastic Syndromes
Myelodysplastic syndromes (MDS) are conditions that can occur when the blood-forming cells in the bone marrow become abnormal. This leads to low numbers of one or more types of blood cells.
Signs and Symptoms :
People with myelodysplastic syndromes might not experience signs and symptoms at first.
- Fatigue
- Shortness of breath
- Pallor due to anemia
- Easy or unusual bruising or bleeding, which occurs due to a low blood platelet count (thrombocytopenia)
- Pinpoint-sized red spots just beneath the skin that are caused by bleeding (petechiae)
- Frequent infections, which occur due to a low white blood cell count (leukopenia)
Types of myelodysplastic syndromes:
Myelodysplastic syndromes with single-lineage dysplasia:
One blood cell type — white blood cells, red blood cells or platelets — is low in number and appears abnormal under the microscope.
Myelodysplastic syndromes with multilineage dysplasia:
Two or three blood cell types are abnormal.
Myelodysplastic syndromes with ring side blasts:
This subtype involves a low number of one or more blood cell types. A characteristic feature is that existing red blood cells in the bone marrow contain rings of excess iron.
Myelodysplastic syndromes with isolated del(5q) chromosome abnormality:
People with this subtype have low numbers of red blood cells, and the cells have a specific mutation in their DNA.
Myelodysplastic syndromes with excess blasts:
In this subtype, any of the three types of blood cells — red blood cells, white blood cells or platelets — might be low and appear abnormal under a microscope. Very immature blood cells (blasts) are found in the blood and bone marrow.
Myelodysplastic syndromes, unclassifiable:
There are reduced numbers of one or more types of mature blood cells and the cells might look abnormal under the microscope, the blood cells appear normal, but analysis might find that the cells have DNA changes that are associated with myelodysplastic syndromes.
Diagnosis :
💢Blood studies
💢Bone marrow analysis
Treatment:
Management of myelodysplastic syndromes is most often intended to slow the disease, ease symptoms and prevent complications. There's no cure for myelodysplastic syndromes, but some medications can help slow the progression of the disease.
Blood transfusions:
Blood transfusions with healthy blood cells from donors can be used to replace red blood cells and platelets in people with myelodysplastic syndromes. Blood transfusions can help control symptoms.
Medications:
Treatment for myelodysplastic syndromes might include medications that:
- Increase the number of blood cells
- Stimulate blood cells to mature.
- Suppress your immune system
- Help people with a certain genetic abnormality
- Treat infections.
Bone marrow transplant:
A bone marrow transplant, also known as a stem cell transplant, is the only treatment option that offers the potential of a cure for myelodysplastic syndromes.
But this treatment carries a high risk of serious complications and it's generally reserved for people who are healthy enough to endure it.
Myeloproliferative Neoplasms
Myeloproliferative neoplasms (MPNs) are types of blood cancer that begin with an abnormal mutation in a stem cell in the bone marrow. The change leads to an overproduction of any combination of white cells, red cells and platelets.
Myeloproliferative neoplasm types:
There are several types of myeloproliferative neoplasms.
Primary myelofibrosis:
- Affects the red blood cells and granulocytes, a type of white blood cell. The cells don't mature normally and are irregularly shaped.
- Primary myelofibrosis also causes thickening or scarring of the fibers inside bone marrow, which can decrease the production of red blood cells and cause anemia.
Polycythemia vera :
- Caused by the overproduction of red blood cells in the bone marrow, which then build up in the blood.
- The spleen swells as extra blood cells collect there, causing pain or a full feeling on the left side. Itching all over the body is a symptom of PV.
Essential Thrombocythemia:
- Number of platelets in the blood is much higher than normal, while other blood cell types are normal.
Chronic eosinophilic leukemia/hyper eosinophilic syndrome:
- Characterized by a higher than normal number of the white blood cells responsible for fighting allergic reactions and some parasitic infections.
Systemic mastocytosis:
- Affects mast cells which are found in skin, connective tissue and in the lining of the stomach and intestines.
- Mast cells serve as a sort of alarm system by signaling disease-fighting blood cells to target areas of the body where they're needed.
- They may also play a role in wound healing.
- SM is caused by too many mast cells accumulating in the body's tissues, which can eventually affect the spleen, bone marrow, liver or small intestine.

References:
1.McCance K.L. & Huether, S.E., (2019). Pathophysiology: The biologic basis for disease in adults and children. 8th ed. Elsevier. St Louis
4.https://www.mayoclinic.org/diseases-conditions/acute-lymphocytic-leukemia/diagnosis-treatment/drc-20369083
5.https://www.cancer.org/cancer/hodgkinlymphoma.html































Comments
Post a Comment